
For You And Your Baby
Written by Nicole Tomazic-Spanger
I took prenatal vitamins religiously throughout both my pregnancies. While I knew that I might be deficient in some nutrients, I began my staple during the preconception period specifically to increase folic acid. I was fortunate to birth two healthy children, but in retrospect, I wish that I had taken prenatal vitamins that were better suited to my individual needs, rather than assuming that they are all the same.
Folate vs Folic Acid
Chemists set out to create a synthetic version of folate in 1931, after concluding that anaemia was caused by a deficiency in B vitamins. Until then, humans had always received vitamin B9 directly from their food. In 1941, the new supplement, folic acid was introduced to the market, as a replacement for naturally occurring folate. Since then, the media and government bodies have used the terms folic acid and folate interchangeably. This confusion in terminology has to lead to the commonly held belief that folate and folic acid are the same compounds, but they’re not.
Folate
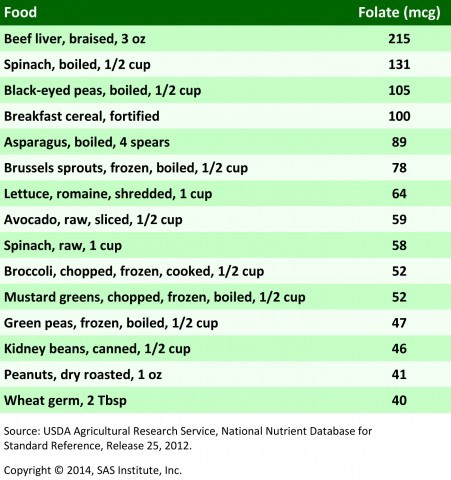
Folate is naturally occurring water-soluble Vitamin B9, and it is found in foods such as leafy green vegetables, broccoli, peas, corn, cereal and meats such as liver and poultry, as well as citrus fruits. Folate deficiency is linked to anaemia, depression and fatigue, as well as many other health-related problems. The benefits of naturally occurring dietary folate in pregnancy and preconception include birth defect prevention, improvement of adequate birth weight, and healthy neural tube formation in early embryo development. The recommended daily intake of folate during pregnancy is 600 mcg a day. The non-pregnant recommendation is 400 mcg a day. The following graph breaks down foods containing folate to achieve the recommended daily intake.
Folic Acid
While folate is naturally occurring, folic acid is man-made. Folic acid is the synthetic B vitamin form and is the inactive form of folate. Folic acid is found in synthetic supplements and also in fortified foods. A mandatory national fortification program of folic acid in our foods means that we no longer have a choice whether to include this supplement in our diets or not. Because neural tubes form early in pregnancy, any deficiencies in folate must be corrected prior to conception. To protect the population, in 1995, national public health policies made it mandatory for Australian millers to include folic acid in wheat flour and grain-based baked goods. Some breakfast cereal manufacturers have also opted to include folic acid in their products for marketing purposes. As a result of compulsory fortification of folic acid in foods, incidents of neural tube defects have substantially reduced.
The Overconsumption Of Folic Acid
The mandatory inclusion of folic acid in some foods, combined with the way in which the body metabolizes folic acid supplements can lead to excessive human consumption. Natural folates are easily metabolized to tetrahydrofolic acid in the lining of the small intestine and are then available to be utilized by the body. Folic acid, on the other hand, must be processed in the liver and there it relies on the enzyme dihydrofolate reductase to break it down and convert it to tetrahydrofolic acid. Unfortunately, this enzyme is not efficient and does not make adequate amounts. When people consume large amounts of folic acid in supplements or in fortified foods, the body then struggles to break it down, and so it doesn’t get converted into tetrahydrofolic acid, instead of entering the bloodstream as excess, un-metabolized folic acid.
Excess Folic Acid and Links To Cancer
In Nature magazine, scientists warned in 2005 that the use of folic acid in fortified foods could have “the side effect of increasing the prevalence of some of the most significant, human life-threatening diseases.” More recent studies have shown that overconsumption of folic acid in the body is linked with an increased risk of cancer. Cornelia M. Ulrich from the Fred Hutchinson Cancer Research Center states that “Although increases in folate before the existence of preneoplastic lesions (such as aberrant crypt foci or polyps in the colon) can prevent tumour development, supplementation with synthetic folic acid may enhance progression once preneoplastic lesions are present.” A randomized controlled trial concluded that supplementing with folic acid presented an increased risk of cancer, and Ulrich states that “These results suggest that the role of folate in fostering the growth of pre-cancerous cells is a real concern for humans at intakes that can be achieved with a combination of supplement use and fortification with folic acid.”
Conversion Of Folic Acid and The MTHFR Defect
It is estimated that approximately 50% of the population have a genetic defect called MTHFR (Methylene-TetraHydroFolate Reductase). Recently, through blood testing, I learned that I am one of these people. MTHFR is a crucial enzyme that is responsible for converting natural dietary folate into the active form called 5-Methylfolate, which is important for many of the body’s functions.
The inability to convert folic acid into a useable form during pregnancy is particularly concerning. This unusable folic acid builds up from both fortified foods and prenatal supplements and can cause both toxicity and folate deficiency because it blocks the absorption of naturally occurring folate. Folate deficiencies are associated with some birth defects. In people with this defect, the supplemental forms of folic acid, as well as folate enriched foods, should be avoided altogether, because the MTHFR mutation has partially destroyed the MTHFR enzyme, responsible for processing folic acid. Mandatory inclusion of folic acid in foods, and blanketed marketing makes this difficult.
During the preconception period, a simple blood test will show the MTHFR status of the individual. This test can be arranged via your GP of directly through an organization called MTHFR Australia. It is crucial for women to know their MTHFR status prior to supplementing with folic acid, and having this knowledge earlier, would have equipped me to have made a better choice of prenatal vitamins for my babies and my own body.
Alternatives to Folic Acid
An alternative to Folic acid is folinic acid, also referred to as methyfolate or 5-MTHFR. This is an active form of folic acid which is already methylated and is available over the counter. This is the safer option for people in this MTHFR positive category to take, such as myself. A variety of prenatal vitamin blends exist on the market, which is specifically designed to bypass the MTHFR gene. Seeking Health Optimal Prenatal by MTHFR expert, Dr Ben Lynch contains methylfolate and folinic acid, perfect for women who cannot process folic acid.
Making The Right Choice For You And Your Baby
While a personalised medical approach to prenatal vitamins is not commonplace yet, hopefully, there will eventually be a move away from the one size fits all approach. Before selecting the right prenatal supplement for you and your baby, it is important to gauge which minerals you are deficient in, and which nutrients you do not need to supplement. Each prenatal blend includes or omits different minerals, or contain ingredients of different strengths. For example, Optimal Prenatal does not include iron, and so it may be necessary to add a second vitamin if there is an existing deficiency in your case. Talking to your doctor, examining the ingredients list, and arranging a blood test hair tissue mineral analysis can be useful in making an informed decision.
Mothers will continue to be deficient in some vitamins and minerals prior to conception. Therefore, prenatal vitamins continue to be an important consideration for a healthy pregnancy. It is up to each individual, however, to ensure that both baby and mother are protected; and to ensure that neither of them is compromised in this process.
How To Choose How To Choose How To Choose How To Choose How To Choose How To Choose How To Choose




1 Comment